Shift work, long working hours, occupational stress, high work intensity, and low healthcare worker-to-population ratios are common among healthcare workers, and these factors often negatively impact their psychosomatic health, including the development of psychological stress and somatic pain[1-2]. These conditions are not only a problem for individual health, but also constitute a major public health issue[3]. A Meta-analysis has indicated that anxiety is the most commonly reported psychological stress reaction among healthcare workers[4]. Several studies[5-7] conducted in China have shown that the prevalence of anxiety among medical staff ranges from 11.4% to 41.1%.
Furthermore, studies[8-9] have shown that, due to the high-intensity workloads, healthcare workers commonly experience somatic pain, and this pain can further exacerbate psychological stress reactions. It has been found that individuals experiencing somatic pain are at a higher risk of developing anxiety compared to the general population[10].
Psychological resilience refers to a person’s ability to quickly adapt and return to a state of equilibrium when faced with stress, frustration, and adversity[11]. Research has demonstrated that increased psychological resilience enables healthcare workers to mitigate negative emotions such as anxiety while enhancing their productivity and work quality in demanding work environments[12]. Additionally, individuals with higher levels of resilience may experience less mood disturbance under somatic pain[13].
It is a noteworthy fact that healthcare workers frequently experienced sleep disturbances[14]. However, good sleep contributes to an individual’s psychological resilience[15]. In contrast, individuals with poor sleep quality have a poor psychological stress capacity, which increases the likelihood of anxiety[16].
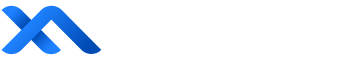
In summary, healthcare workers face the dual challenge of somatic pain and anxiety symptoms[13]. Current knowledge suggests that higher levels of psychological resilience are a potential protective factor against anxiety symptoms, though this protection can be influenced by sleep disorders[13, 15]. However, the current study has not been able to confirm the above hypotheses and the applicability to medical staff has not been fully explored. Therefore, we proposed the following hypotheses (Figure 1): 1) Psychological resilience may mediate the relationship between somatic pain and anxiety. 2) Sleep plays a moderating role in the relationship between psychological resilience and anxiety.
This study aims to examine the potential mediating effects and discuss the development of targeted psychological interventions for medical personnel. The findings of this research may have implications for promoting rational health practices for both medical institutions and healthcare workers, including education and intervention about sleep and psychological resilience.
Materials and Methods
Study
Participants were recruited through convenience sampling in February 2023 at the The Second Xiangya Hospital of Central South University, and an online questionnaire survey was conducted among healthcare workers. Participation was voluntary, and informed consent was obtained at the beginning of the survey after providing a brief introduction to the study’s content and purpose. Incomplete answers for any question were excluded, only fully completed questionnaires were included in the final statistical analysis. The final sample consisted of 1 661 individuals.
Methods
Demographic characteristics
A self-designed questionnaire was used to collect demographic information from healthcare workers, including gender, age, job position, occupation, professional title, years of work, education, whether their current job is related to COVID-19, and the duration of their participation in COVID-19-related work. We integrated the above information into 5 covariates, which were later categorized. In this study, gender was classified as male and female; age in years was classified into 18-30 years, 31-40 years, 41-50 years, 51 years and above; education was classified as specialized and below, undergraduate, postgraduate student, doctor and above; years of experience was classified into <2 years, 3-5 years, 6-10 years, >10 years; position in pandemic was classified as ICU/critical care areas, general ward for COVID-19, Emergency, other wards.
Visual Analogue Scale
A Visual Analogue Scale (VAS) was used to assess somatic pain. The VAS is a simple and rapid measure of subjective pain intensity that has been widely used in various populations, including patients with major depressive disorder experiencing somatic symptoms. It utilizes a scoring ranging from 0 to 10, with higher scores indicating greater pain intensity[17].
Generalized Anxiety Disorder-7 questionnaire
The Generalized Anxiety Disorder-7 (GAD-7) is a 7-item screening measure used to assess symptoms of generalized anxiety over the past 2 weeks[18]. Participants were asked to rate the frequency of experiencing symptoms described in each item on a 4-point Likert scale ranging from 0 (not at all) to 3 (nearly every day). The GAD-7 has been widely tested and used, with the reliability and validity of the Chinese version documented in Chinese general hospital patients[19]. In previous research, a cut point of 5 can be interpreted as representing mild levels of anxiety[18, 20]. The internal consistency of the scale in this study was 0.940.
Psychological resilience assessment
Psychological resilience was assessed through the 10-item Connor-Davidson Resilience Scale (CD-RISC-10). The CD-RISC-10 is a self-report measure consisting of 10 items used to assess psychological resilience, defined as the ability to cope with adversity[21]. Each item on the CD-RISC-10 is scored on a 5-point Likert scale, ranging from 0 (not true at all) to 4 (true nearly all the time). The total score on the CD-RISC-10 ranges from 0 to 40, with higher scores indicating a higher level of resilience[22-23]. In this study, the internal consistency of the CD-RISC-10 was considered excellent, with a Cronbach’s α of 0.965 calculated.
Sleep disturbance assessment
Sleep disturbance was assessed through the Q3 item of Patient Health Questionnaire-9 Items, (PHQ-9). We utilized one question for sleep disturbance (Q3: Over the last 2 weeks, how often have you been bothered by the following problems: trouble falling or staying asleep, or sleeping too much?) from the PHQ-9[24]. Responses were scored on a 4-point scale (0 for “never”, 3 for “almost daily”). Higher Q3 scores indicate greater sleep disturbance.
Statistical analyses
For data processing, this study employed Statistical Product and Service Solutions (SPSS) version 26.0. Principal component analysis was used to evaluate common method bias[25]. Covariate tests derived from demographic information were conducted using χ2 tests, with statistically significant variables being considered as confounders and included in the analysis of mediating effects. Pearson correlation analyses were conducted to examine the correlations among the predictors in this study, and the mediating effect hypothesis was built upon the results of the correlation analysis.
In order to investigate the mediating effects, we employed “Model 4” and “Model 14” of the PROCESS macro program, implementing the bootstrap method. To examine the mediating effect of psychological resilience between somatic pain and anxiety symptoms, we utilized Model 4 in the PROCESS macro program to estimate 95% confidence intervals (CI) for the mediating effect through 5 000 iterations of Bootstrap sampling. The mediation effect tests were conducted with somatic pain as the independent variable, psychological resilience as the mediator variable, and anxiety symptoms as the dependent variable[26]. Furthermore, to analyze the mediating role of sleep disturbance between psychological resilience and anxiety symptoms, we used Model 14 of the PROCESS macro program for regression analysis. P<0.05 was considered statistically significant.
Results
Control and test of common method deviation
The common method bias test was performed by Harman single factor method, taking the characteristic root greater than 1 as the standard. The results showed that the exploratory factor analysis extracted 2 factors with a characteristic root greater than 1, and the first factor explained 46.62% of the total variance (<50%). Therefore, this study can be considered that there is no obvious common method bias.
Descriptive statistics
A total of 1 661 participants were included in this study, consisting of 213 (12.82%) males and 1 448 (87.18%) females. Using a cutoff point of 5 for the GAD-7 scale, 647 (38.95%) healthcare workers were found to exhibit symptoms of anxiety. There were statistically significant differences in all covariates between the anxiety and non-anxiety groups (all P<0.05). Using a cutoff point of 20 for psychological resilience, 393 (23.66%) healthcare workers were classified into the low-resilience group, while the remaining participants were in the high-resilience group. Significant differences in gender, age group, and education were observed between the low-resilience and high-resilience groups (P<0.05). Using a cutoff of 4 to determine the severity of somatic pain, 681 (41.00%) participants reported experiencing severe somatic pain. A statistically significant difference in gender was observed between participants reporting mild and severe somatic pain (P<0.05, Table 1).
| Characteristics | No. (%) | Anxiety symptoms/[No. (%)] | P | Psychological resilience/[No. (%)] | P | Somatic pain/[No. (%)] | P | |||
|---|---|---|---|---|---|---|---|---|---|---|
| <5 (n=1 014) | ≥5 (n=647) | <20 (n=393) | ≥20 (n=1 268) | <4 (n=980) | ≥4 (n=681) | |||||
| Gender | 0.003 | 0.005 | <0.001 | |||||||
| Male | 213(12.8) | 150(70.4) | 63(29.6) | 34(16.0) | 179(84.0) | 154(72.3) | 59(27.7) | |||
| Female | 1 448(87.2) | 864(59.7) | 584(40.3) | 359(24.8) | 1089(75.2) | 826(57.0) | 622(43.0) | |||
| Age/year | <0.001 | 0.010 | 0.054 | |||||||
| 18-30 | 419(25.2) | 256(61.1) | 163(38.9) | 117(27.9) | 302(72.1) | 266(63.5) | 153(36.5) | |||
| 31-40 | 702(42.3) | 398(56.7) | 304(43.3) | 173(24.6) | 529(75.4) | 412(58.7) | 290(41.3) | |||
| 41-50 | 320(19.3) | 188(58.8) | 132(41.2) | 64(20.0) | 256(80.0) | 171(53.4) | 149(46.6) | |||
| 51 and above | 220(13.2) | 172(78.2) | 48(21.8) | 39(17.7) | 181(82.3) | 131(59.5) | 89(40.5) | |||
| Education | <0.001 | 0.000 | 0.062 | |||||||
| Specialized and below | 170(10.2) | 133(78.2) | 37(21.8) | 58(34.1) | 112(65.9) | 95(55.9) | 75(44.1) | |||
| Undergraduate | 970(58.4) | 516(53.2) | 454(46.8) | 253(26.1) | 717(73.9) | 553(57.0) | 417(43.0) | |||
| Postgraduate student | 326(19.6) | 228(69.9) | 98(30.1) | 64(19.6) | 262(80.4) | 205(62.9) | 121(37.1) | |||
| Doctor and above | 195(11.8) | 137(70.3) | 58(29.7) | 18(9.2) | 177(90.8) | 127(65.1) | 68(34.9) | |||
| Experience | <0.001 | 0.108 | 0.050 | |||||||
| <2 years | 171(10.3) | 121(70.8) | 50(29.2) | 45(26.3) | 126(73.7) | 116(67.8) | 55(32.2) | |||
| 3-5 years | 168(10.1) | 110(65.5) | 58(34.5) | 46(27.4) | 122(72.6) | 104(61.9) | 64(38.1) | |||
| 6-10 years | 392(23.6) | 201(51.3) | 191(48.7) | 103(26.3) | 289(73.7) | 231(58.9) | 161(41.1) | |||
| >10 years | 930(56.0) | 582(62.6) | 348(37.4) | 199(21.4) | 731(78.6) | 529(56.9) | 401(43.1) | |||
| Position in Pandemic | <0.001 | 0.074 | 0.245 | |||||||
| ICU/critical care areas | 362(21.8) | 162(44.8) | 200(55.3) | 100(27.6) | 262(72.4) | 212(58.6) | 150(41.4) | |||
| General ward for COVID-19 | 484(29.1) | 289(59.7) | 195(40.3) | 120(24.8) | 364(75.2) | 303(62.6) | 181(37.4) | |||
| Emergency | 88(5.3) | 44(50.0) | 44(50.0) | 22(25.0) | 66(75.0) | 48(54.6) | 40(45.4) | |||
| Other wards | 727(43.8) | 519(71.4) | 208(28.6) | 151(20.8) | 576(79.2) | 417(57.4) | 310(42.6) | |||
Correlation analyses
Correlation analysis showed that there were statistically significant correlations between the main predictors in this study (all P<0.05). Among them, Psychological resilience showed negative correlation with sleep disturbance (r=-0.313), anxiety symptoms (r=-0.451), and somatic pain (r=-0.214); anxiety symptoms and sleep disturbance (r=0.638), anxiety symptoms and somatic pain (r=0.344), sleep disturbance and somatic pain (r=0.325) all showed a positive correlation (Table 2).
| Sleep Disturbance | Anxiety Symptoms | Psychological Resilience | Somatic Pain | |
|---|---|---|---|---|
 | 0.84±0.83 | 3.85±4.18 | 25.05±9.40 | 3.07±1.90 |
| Sleep Disturbance | ||||
| Anxiety Symptoms | 0.638** | |||
| Psychological Resilience | -0.313** | -0.451** | ||
| Somatic Pain | 0.325** | 0.344** | -0.214** |
Analysis of moderated mediator
Effect of psychological resilience between somatic pain and anxiety symptoms
The results showed that in Model I, the effect of somatic pain on psychological resilience was statistically significant (β=-0.753, P<0.01); in Model II, when both somatic pain and psychological resilience were included in the regression analyses, the effect of both somatic pain (β=12.620) and psychological resilience (β=-14.126) on the anxiety symptoms was statistically significant (P<0.01, Table 3).
| Model | Predictor | Outcome | R | R2 | β | LLCI | ULCI | t |
|---|---|---|---|---|---|---|---|---|
| Model I | Somatic pain | Resilience | 0.237 | 0.056 | -0.753 | -0.987 | -0.519 | -6.307** |
| Model II | Somatic pain | Anxiety | 0.494 | 0.244 | 0.608 | 0.513 | 0.702 | 12.620** |
| Resilience | — | — | — | -0.138 | -0.158 | -0.119 | -14.126** | |
| Model III | Somatic pain | Anxiety | 0.391 | 0.153 | 0.712 | 0.613 | 0.818 | 14.137** |
The interaction term between somatic pain and psychological resilience (results of path analysis) indicated that the mediating effect of psychological resilience between somatic pain and anxiety levels was statistically significant (Table 4).
| Effect Type | Effect value | Boot SE | 95% CI | Relative effect size/% |
|---|---|---|---|---|
| Total effect | 0.712 | 0.050 | 0.613-0.811 | — |
| Direct effect | 0.608 | 0.048 | 0.513-0.702 | 85.39 |
| Mesomeric effect | 0.104 | 0.022 | 0.066-0.150 | 14.61 |
Effect of sleep disturbance between psychological resilience and somatic pain
The results showed a statistically significant effect of the interaction between sleep disturbance and psychological resilience on anxiety symptoms (β=-0.103, P<0.01; Table 5).
| Predictor | Psychological resilience | Anxiety symptoms | ||||
|---|---|---|---|---|---|---|
| β | SE | t | β | SE | t | |
| Somatic pain | -0.753 | 0.119 | -3.656 | 0.254 | 0.041 | 6.231** |
| Resilience | — | — | — | -0.116 | 0.008 | -13.995** |
| Sleep disturbance | — | — | — | 2.440 | 0.096 | 25.401** |
| Resilience & Sleep | — | — | — | -0.103 | 0.010 | -10.803** |
| R2 | 0.056 | 0.507 | ||||
| F | 16.358** | 188.694** | ||||
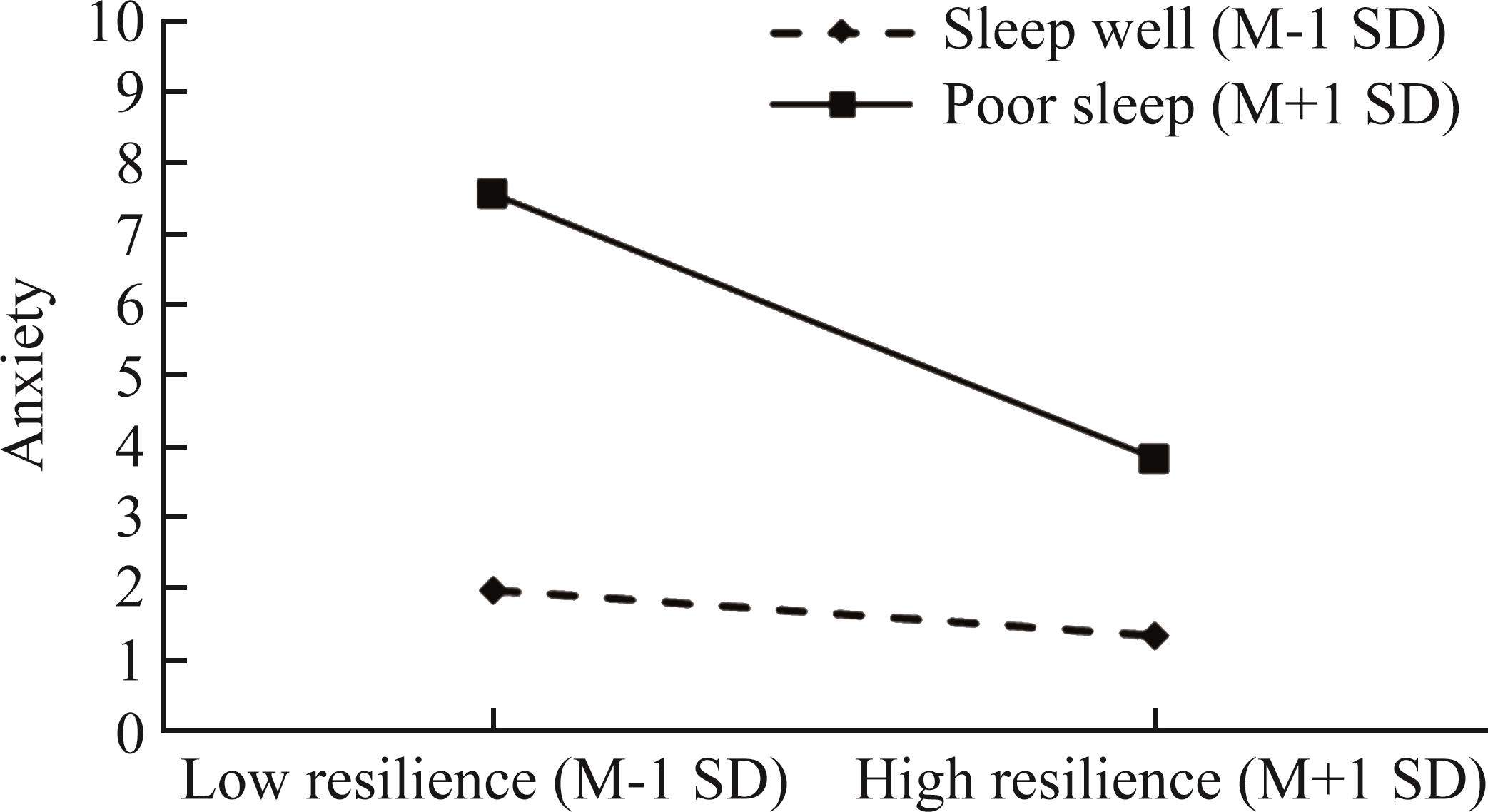
In order to visualize the effect of sleep disturbance moderating psychological resilience on anxiety symptoms, we grouped the values of sleep disturbance scores in high and low groups at ± standard deviation (±1 SD) and performed a simple slope effect analysis. The results showed that sleep disturbance had a moderating on the relationship between psychological resilience and anxiety symptoms (Figure 2).
Discussion
In this study, the prevalence of anxiety symptoms was 38.95%. Notably, this prevalence rate is higher than the findings reported in a previous study conducted by Wang, et al[27] in 2022 among Chinese healthcare workers, where the prevalence of anxiety symptoms was reported to be 24.4%. This difference can be attributed to various factors, such as the unique working environment, particularly the complete lifting of pandemic control measures, which has resulted in an enormous workload for healthcare workers, along with the ongoing risk of infection. The participants in this phase may have experienced heightened levels of stress compared to the control phase, which subsequently impacted their anxiety levels[28].
Medical personnel have long hours and heavy workloads, because they often work overtime, yet there are some imbalances in terms of effort and reward[29]. In addition, due to the large population, healthcare workers have to serve more patients compared to other developed countries. Finally, the relationship between healthcare workers and patients is very tense, which may also contribute to healthcare workers’ anxiety[30]. In conclusion, these facts show that medical personnel have more chances to face illness and death, which negatively affects their mental health.
Psychological resilience was found to have a significant negative correlation with the risk of anxiety, consistent with the findings of Moritz, et al[31]. In a work environment where pandemic control measures have been fully lifted, healthcare workers with higher psychological resilience exhibit better adaptability, leading to reduced stress responses and lower levels of anxiety.
Furthermore, anxiety symptoms were observed to have a significant negative correlation with psychological resilience, aligning with the findings of Lyon, et al[32-33]. Anxiety lowers the level of psychological resilience among healthcare workers, impairing their ability to regulate their adaptive capacity when faced with significant stressors, thus hindering their quick recovery.
Moreover, a significant negative correlation was identified between sleep disturbance and psychological resilience, corresponding to the findings of Tu, et al[34]. Medical personnel with better sleep quality demonstrate higher scores of psychological elasticity and stronger psychological resilience, enabling them to effectively manage stress and cope with demanding workloads in a high-intensity setting.
This study revealed a mediating role of psychological resilience between somatic pain and anxiety symptoms. The findings indicate that somatic pain among healthcare workers positively influences anxiety levels, and this effect can be indirectly mediated by psychological resilience. A high level of psychological resilience often acts as a buffer against the negative impact of somatic pain. In other words, medical workers experiencing somatic pain but possessing good psychological resilience are typically more adept at regulating their emotions and adjusting their work status accordingly. Heightened anxiety levels may amplify the experience of pain, making it more intense or persistent. Resilient individuals tend to exhibit more adaptive responses to stressors, which can buffer the relationship between anxiety and physical pain and enhance an individual’s capacity to employ effective coping strategies[22], potentially reducing the influence of anxiety on the perception and experience of physical pain.
This study also explored the mediating role of sleep disturbance in the hypothesized model. The results indicate that sleep disturbance moderates the latter part of the proposed model, specifically the relationship between psychological resilience and anxiety levels. Sleep, being a normal physiological process, mitigates the risk of anxiety symptoms associated with lower psychological resilience. Psychological resilience often mitigates the perception of physical pain. Individuals with higher resilience might exhibit better coping mechanisms, reducing the impact of pain on their overall well-being[22]. Adequate sleep contributes to emotional regulation and resilience. It enables individuals to manage stress more effectively and enhances their ability to cope with adversity and recover from challenges[35].
In summary, the relationship between psychological resilience and anxiety is strengthened when sleep disturbance is intensified. As psychological resilience decreases, healthcare workers become more susceptible to anxiety. Conversely, for healthcare workers with better sleep, the impact of psychological resilience on anxiety is weakened, resulting in lower anxiety levels. Thus, it is crucial to address sleep deprivation and improve sleep quality for healthcare workers in order to promote better mental well-being.
The findings of this study have significant implications for enhancing the psychological resilience of healthcare workers and mitigating their anxiety levels in the face of sudden and intense workloads in the future. Conducting early assessments among medical personnel to detect sleep problems, mental health issues, and physical discomfort, along with implementing effective intervention strategies for these problems, is crucial. Additionally, timely intervention to address serious negative thoughts experienced by medical staff can help reduce adverse mental health outcomes[36]. Furthermore, it is essential to provide care for healthcare workers and implement interventions aimed at improving their psychological resilience. Studies[3, 37] suggests that social support is critical to increasing psychological resilience, and that strengthening emotional regulation or providing psychotherapy may help to increase their resilience. This will enhance their adaptability and promote their physical and mental well-being recovery. Additionally, improving sleep quality for medical staff can play a role in alleviating anxiety and should be considered as an intervention to reduce anxiety levels. The best way to improve one’s sleep is to maintain sleep hygiene by changing one’s sleep habits. Good sleep hygiene practices can promote better quality and duration of sleep and have significant physical and psychological benefits[38].
There are several limitations to this study. First, sleep disturbance in this study was assessed with only one question, which may have led to under-representation. In subsequent studies, sleep status could be taken to a better questionnaire to increase the confidence of the findings. Second, covariate inclusion could have been more. Finally, the surveys and scales we used in this study were based on respondents’ self-reports, which reflect only subjective evaluations, and future studies based on objective evaluations could be conducted.
抗疫一线医护人员团队复原力、社会支持与心理健康的关系: 个人复原力的中介作用
[J]. 中国临床心理学杂志, 2020, 28(4): 747-750, 729. https://doi.org/10. 16128/j.cnki.1005-3611.2020.04.020.The association between psychological strains and life satisfaction: evidence from medical staff in China
[J]. J Affect Disord, 2020, 260: 105-110. https://doi.org/10.1016/j.jad.2019.09.006.Mediation effect of perceived social support and psychological distress between psychological resilience and sleep quality among Chinese medical staff
[J]. Sci Rep, 2024, 14(1): 19674. https://doi.org/10.1038/s41598-024-70754-3.The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public—A systematic review and Meta-analysis
[J]. Psychiatry Res, 2020, 291: 113190. https://doi.org/10. 1016/j.psychres.2020.113190.The prevalence and influencing factors in anxiety in medical workers fighting COVID-19 in China: a cross-sectional survey
[J]. Epidemiol Infect, 2020, 148: e98[Job burnout and anxiety among medical staff: a latent profile and moderated mediation analysis
[J]. Soc Sci Med, 2024, 356: 117141. https://doi.org/10.1016/j.socscimed. 2024.117141.Understanding the mediating role of anxiety and depression on the relationship between perceived stress and sleep quality among health care workers in the COVID-19 response
[J]. Nat Sci Sleep, 2021, 13: 1747-1758. https://doi.org/10.2147/NSS.S313258.The COVID-19 pandemic and its consequences for chronic pain: a narrative review
[J]. Anaesthesia, 2022, 77(9): 1039-1050. https://doi.org/10. 1111/anae.15801.Chronic pain: an update on burden, best practices, and new advances
[J]. Lancet, 2021, 397(10289): 2082-2097. https://doi.org/10.1016/S0140-6736(21)00393-7.Neurocognitive dysfunctioning and the impact of comorbid depression and anxiety in patients with somatic symptom and related disorders: a cross-sectional clinical study
[J]. Psychol Med, 2018, 48(11): 1803-1813. https://doi.org/10.1017/S0033291717003300.Coping and life satisfaction: mediating role of ego-resiliency in patients with rheumatoid arthritis
[J]. Med Princ Pract, 2020, 29(2): 160-165. https://doi.org/10.1159/000503708.初入高原工作的医务人员不同应对方式与焦虑抑郁的关系以及心理弹性的中介作用
[J]. 中华全科医学, 2022, 20(8): 1367-1371. https://doi.org/10.16766/j.cnki.issn.1674-4152.002599.The role of resilience, happiness, and social support in the psychological function during the late stages of the lockdown in individuals with and without chronic pain
[J]. Int J Environ Res Public Health, 2022, 19(11): 6708. https://doi.org/10.3390/ijerph19116708.The prevalence of sleep disturbances among physicians and nurses facing the COVID-19 patients: a systematic review and meta-analysis
[J]. Global Health, 2020, 16(1): 92. https://doi.org/10.1186/s12992-020-00620-0.Exploring the bi-directional relationship between sleep and resilience in adolescence
[J]. Sleep Med, 2020, 73: 63-69. https://doi.org/10. 1016/j.sleep.2020.04.018.Psychological resilience mediates the association between sleep quality and anxiety symptoms: a repeated measures study in college students
[J]. PLoS One, 2023, 18(10): e0292887[Measures of adult pain: visual analog scale for pain (VAS pain), numeric rating scale for pain (NRS pain), McGill pain questionnaire (MPQ), short-form McGill pain questionnaire (SF-MPQ), chronic pain grade scale (CPGS), short form-36 bodily pain scale (SF-36 BPS), and measure of intermittent and constant osteoarthritis pain (ICOAP)
[J]. Arthritis Care Res, 2011, 63(A brief measure for assessing generalized anxiety disorder: the GAD-7
[J]. Arch Intern Med, 2006, 166(10): 1092-1097. https://doi.org/10. 1001/archinte.166.10.1092.Generalized anxiety disorder in urban China: prevalence, awareness, and disease burden
[J]. J Affect Disord, 2018, 234: 89-96. https://doi.org/10.1016/j.jad. 2018.02.012. https://doi.org/10.1016/j.jad.2022.12.152Mental condition and function of resilience among families of frontline medical workers during COVID-19: potential influencing factors and mediating effect
[J]. J Affect Disord, 2023, 324: 600-606. https://doi.org/10.1016/j.jad.2022.12.152.Development of a new resilience scale: the connor-Davidson resilience scale (CD-RISC)
[J]. Depress Anxiety, 2003, 18(2): 76-82. https://doi.org/10.1002/da. 10113.Psychometric analysis and refinement of the connor-Davidson resilience scale (CD-RISC): validation of a 10-item measure of resilience
[J]. J Trauma Stress, 2007, 20(6): 1019-1028. https://doi.org/10.1002/jts.20271.Examination of the Connor-Davidson Resilience Scale 10 (CD-RISC-10) using the polytomous Rasch model
[J]. Psychol Assess, 2021, 33(7): 672-684. https://doi.org/10.1037/pas0001011.The PHQ-9: validity of a brief depression severity measure
[J]. J Gen Intern Med, 2001, 16(9): 606-613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x.共同方法偏差检验: 问题与建议
[J]. 心理科学, 2020, 43(1): 215-223. https://doi.org/10.16719/j.cnki.1671-6981.20200130.国内中介效应的方法学研究
[J]. 心理科学进展, 2022, 30(8): 1692-1702. https://doi.org/10.3724/SP. J.1042.2022.01692.A cross-sectional study of the psychological status of 33, 706 hospital workers at the late stage of the COVID-19 outbreak
[J]. J Affect Disord, 2022, 297: 156-168. https://doi.org/10.1016/j.jad.2021.10.013.Depression and anxiety during COVID-19
[J]. Lancet, 2022, 399(10324): 518. https://doi.org/10.1016/S0140-6736(22)00187-8.Serial multiple mediation of organizational commitment and job burnout in the relationship between psychological capital and anxiety in Chinese female nurses: a cross-sectional questionnaire survey
[J]. Int J Nurs Stud, 2018, 83: 75-82. https://doi.org/10.1016/j.ijnurstu.2018. 03.016.医务人员看待精神疾病态度与医患关系和抑郁焦虑水平关系的网络分析
[J]. 中南大学学报(医学版), 2023, 48(10): 1506-1517. https://doi.org/10.11817/j.issn.1672-7347.2023.230115.Risk, resilience, psychological distress, and anxiety at the beginning of the COVID-19 pandemic in Germany
[J]. Brain Behav, 2020, 10(9): e01745[Big Five personality facets explaining variance in anxiety and depressive symptoms in a community sample
[J]. J Affect Disord, 2020, 274: 515-521. https://doi.org/10.1016/j.jad.2020.05.047.Mediating effect of resilience on association among stress, depression, and anxiety in Indonesian nursing students
[J]. J Prof Nurs, 2021, 37(4): 706-713. https://doi.org/10.1016/j.profnurs.2021.04.004.睡眠与认知功能的关系: 心理弹性和抑郁倾向的中介作用
[J]. 中国健康心理学杂志, 2022, 30(9): 1285-1290. https://doi.org/10.13342/j.cnki.cjhp.2022.09.002.The sleep response to stress: how sleep reactivity can help us prevent insomnia and promote resilience to trauma
[J]. J Sleep Res, 2023, 32(6): e13892[The relations between emotion regulation, depression and anxiety among medical staff during the late stage of COVID-19 pandemic: a network analysis
[J]. Psychiatry Res, 2022, 317: 114863. https://doi.org/10.1016/j.psychres.2022.114863.Feasibility, acceptability, and efficacy of a positive emotion regulation intervention to promote resilience for healthcare workers during the COVID-19 pandemic: a randomized controlled trial
[J]. PLoS One, 2024, 19(6): e0305172[Sleep physiology, pathophysiology, and sleep hygiene
[J]. Prog Cardiovasc Dis, 2023, 77: 59-69. https://doi.org/10.1016/j.pcad.2023.02.005.The authors declare that they have no conflicts of interest to disclose.
张悦欣, 莫鸿飞, 唐婧琼, 冯志凌, 喻孟强. 基于医务人员睡眠和心理弹性的横断面研究[J]. 中南大学学报(医学版), 2024, 49(10): 1556-1565. DOI:10.11817/j.issn.1672-7347.2024. 240137
ZHANG Yuexin, MO Hongfei, TANG Jingqiong, FENG Zhiling, YU Mengqiang. A cross-sectional study based on sleep and psychological resilience among medical staff[J]. Journal of Central South University. Medical Science, 2024, 49(10): 1556-1565. DOI:10.11817/j.issn.1672-7347.2024.240137
http://xbyxb.csu.edu.cn/xbwk/fileup/PDF/2024101556.pdf
http://dx.chinadoi.cn/10.11817/j.issn.1672-7347.2024.240137